Veterans Try To Educate Providers on Gulf War Illnesses

By Debbie Gregory.
Servicemembers who deployed for Operation Desert Storm and Operation Desert Shield suffer from an amalgam of chronic, unexplained illnesses including fibromyalgia, fatigue and gastrointestinal disorders, called, for lack of a better name, Gulf War Illness (GWI.)
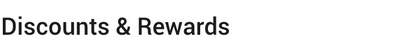
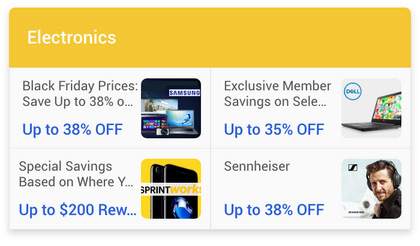
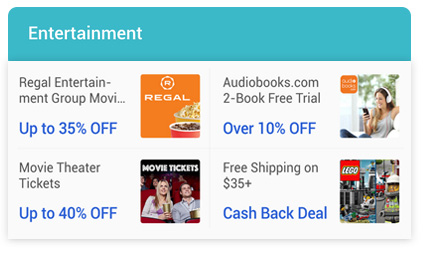
Gulf War veterans may be eligible for a variety of VA benefits, including a Gulf War Registry health exam, the Airborne Hazards and Open Burn Pit Registry, health care, and disability compensation for diseases related to military service. Their dependents and survivors also may be eligible for benefits.
Unfortunately, when a veteran has symptoms suggestive of GWI, the type of care they get may depend on the type of doctor they see. General internal medicine doctors are more likely to believe the syndrome is caused by mental illness. Many physicians don’t even seem to know what GWI is.
This led Shawn Scott to his present cause. Scott suffers from many medical conditions linked to his service. He is on a quest to bridge the information gap. To that end, the Army veteran organized a Gulf War Illness Awareness Conference at his local VA hospital in Tampa, FL.
He has also been a part of a research study conducted by Nancy Klimas and James Baranuiuk, who have made breakthrough discoveries about Gulf War service and GWI.
After Klimas spoke about the GWI clinical trials she’s working on, veterans in attendance at the conference flooded her table with interest.
Although more evidence might not lead to a cure, Klimas is none the less working toward one. At the very least, it could lead to a better understanding and improved treatment for veterans’ symptoms.
Military Connection salutes and proudly serves veterans and service members in the Army, Navy, Air Force, Marines, Coast Guard, Guard and Reserve, and their families.




 By
By