Art Therapy in the Military Community
Art Therapy in the Military Community
Contributed by Alan Rohlfing
In the summer of 2018, I started down a new path. I was never one to avoid technology, but as a crusty old artilleryman, I would rather send high explosive artillery rounds downrange using charts and darts than the automated indirect fire systems we were fielding on a regular basis. But this time, I was fresh to the engagement app scene, helping our little company use the web and social media to make connections and make a difference.
And, a little over a year ago, I wrote an article for our blog called The Healing Power of Art, where I barely skimmed the surface…of how therapeutic art can be. To help dial in and, at the very least, pen a good article, I had to dig in and get my boots muddy. I was fortunate to find a very talented and very giving subject matter expert right here in St. Louis, a 20-year US Navy Submarine Veteran who has both passion and determination to go along with his artistic talent.
That submariner is Scott Beaty, a man for whom the visual arts have long been a format for creative expression, emotional healing, strength, and a sense of purpose. Shortly after he retired from the Service, Scott realized his love for art was also a gateway to his own healing and mental health. Discovering therapy in art, he began pursuing it all the way to earning a Master’s Degree in Fine Art and founding the organization he leads today.
When Scott founded the organization Visions for Vets in 2015, he discovered a way to help Veterans find freedom, purpose, and mental health close to home …through teaching and creating art and building strong Veteran camaraderie. Visions for Vets is a non-profit art school that enriches the lives of military Veterans while empowering them through the healing power of the arts. Based in St. Louis, Missouri, Visions for Vets is an independent non-profit, not affiliated with or funded by any government or VA program. Art as therapy wasn’t necessarily born here, but it sure found a home in Visions for Vets.
Scott talks further about the experience: “We’ve found that once Veterans have gained confidence in their newly-found, rekindled, or enhanced art skills, they’re ready to serve all over again. Service is at the heart of Visions for Vets and we seek to help Veterans continue the mission through art, building important relationships in their communities and engaging in outreach to bring the power of the healing arts to those in need of peace and joy.”
While a tremendous resource for those that need it, Visions for Vets never claims to be an official form of therapy; art therapy is typically facilitated by a professional art therapist to support personal and relational treatment goals as well as community concerns. Art therapists are master-level clinicians who work with people of all ages across a broad spectrum of practice. Honoring individuals’ values and beliefs, art therapists work with people who are challenged with medical and mental health problems, as well as individuals seeking emotional, creative, and spiritual growth.
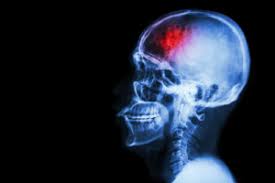
If you’ve seen the healing power of art in action, you know the life-changing effects it can have on our Brothers & Sisters that struggle. Of course, not all Veterans that connect with art have a post-traumatic stress diagnosis, but for those that do, art is a great option for healing. For years, art has been shown to improve interpersonal skills, increase self-awareness, and boost self-esteem. It can mean relief for that PTS and other issues stemming from military service. Clinically speaking, this helps reduce tension and anxiety, which can relieve pain and set a strong foundation for the process of healing or coping with lifelong disabilities. A 2012–14 survey at the National Intrepid Center of Excellence (NICoE, the outpatient clinic dedicated to treatment of Traumatic Brain Injuries at Walter Reed Military Medical Center in Bethesda, Maryland) ranked art therapy among the top five most helpful techniques used to treat veterans.
In addition to Visions for Vets and plenty of other local groups with the same mission, there’s an emphasis on the power of the visual arts at the national level, as well. The Departments of Defense (DoD) and Veterans Affairs (VA) have their own platforms in the Creative Forces Network and the National Veterans Creative Arts Festival.
Creative Forces is a network of caring people made possible by a unique collaboration between the National Endowment for the Arts, DoD, the VA, and state arts agencies; a network made up of creative arts therapists, artists, doctors, military service members, veterans, community leaders, and policymakers who believe in the transformative and restorative powers of art. Those professionals use the creative arts as an effective rehabilitative therapy to help veterans recover from and cope with physical and emotional disabilities by encouraging expression in a non-threatening way. Across the country each year, Veterans enrolled at VA health care facilities compete in local creative arts competitions, culminating in the National Veterans Creative Arts Festival.
So, before you move on to other things, here’s my ‘ask’: connect with the ‘art as therapy’ concept. For those of you looking for a military charity to support, I encourage you to learn more about organizations like Visions for Vets and the people behind them. If you have a battle buddy or know someone else who could benefit from the therapeutic effects of art, help them make the connection. And if it’s you that needs to experience the healing power of art, then by all means, create!